Introduction
Prosthetic rehabilitation using dental implants in edentulous and partially edentulous patients with adequate bone condition is usually a safe treatment with predictable results, showing long term survival rates around 98%. Anatomical limitations, such as reduced bone width and height, generate significant surgical difficulties in the installation of dental implants. In situations involving limited remaining bone, advanced surgical techniques were developed to make possible the installation of the implant, in a simultaneous or staged fashion.
With the development of bone augmentation techniques, it became possible to rehabilitate many of these cases with implant supported prosthesis. However, clinical results show that vertical bone augmentation techniques, such as guided bone regeneration, distraction osteogenesis, interpositional bone grafts, onlay bone grafts, and the use of growth factors, are technique-sensitive. requiring significant surgical experience and producing unpredictable results. Moreover, they also increase treatment time, morbidity, complications, and cost. For the posterior maxilla, the sinus floor elevation is a predictable and well-documented technique, also requires more time and a staged approach in severe atrophies. The vertically deficient posterior mandible remains a challenging anatomic area to restore with implant-supported fixed prosthesis.
In the last decade, the use of short implants (<8mm) became of great interest among professionals. Rehabilitation using short implants in areas with limited bone height Offers a less complex, less costly, and less traumatic treatment for patients. It has been demonstrated by several systematic reviews, RCTs. prospective, and retrospective clinical series publications that the use of short implants is a safer option for edentulous areas with limited bone height, when compared to the advanced and complex vertical augmentation techniques.
Some aspects should be considered of influence in the short- and long-term survival rates of short implants, such as achieving good primary stability, adequate bone to implant contact, potentially a high crown-to-implant ratio, and the effect on the marginal bone loss after loading. Those factors are directly influenced by the implant design, surface, and implant/abutment connection.
The Straumann Dental Implant System (Straumann Group. Basel. Switzerland) has a 6 mm and a 4 mm length implant available, both in the classic Soft-Ttssue Level (STL) level design. The combination of a well-documented surface with a body design aimed at obtaining good primary stability, and a polished collar neck with an internal conical connection, allow this short implant designs to obtain predictable results when addressing the factors above.
Our chapter will discuss characteristics and indications for these two short implants.
The Straumann 6 mm Implant
The utilization of short (6 mm) Straumann implants with the TPS surface goes back to the late-1980s, and favorable clinical results were first reported in the late 1990s. By the end of 1998, the "SLA—Sandblasted Large-Grit, Acid-etched" surface was launched on the 6 mm length and the '*SLActive" surface was made available for the same length by the year 2005. Since then, the Straumann 6 mm implants are available in both "SLA" and "SLActive" surfaces. The SLActive surface brought the possibility of reducing osseointegration time and improving bone to-implant contact. The SLA surface is considered one of the best documented implant surfaces in the market.
Recently, the Roxolid alloy (TIZi) was introduced with improved results not only in the strength of the alloy (it was initially launched with emphasis on reduced diameter implants), but also on the faster and improved osseointegration. It was then expanded to the whole line of the Straumann implants, with both the SLA and SLActive surface treatments.
The Straumann 4 mm Implant
A novel Straumann implant with 4 mm of length (4.1 mm—diameter Straumann Reeular Neck. solid screw. SLActive soft tissue level implants with 0.8-mm thread pitch and 4-mtn length, titanium grade-4) was first introduced in 2009, with some differences from the well-documented 6 mm implant.
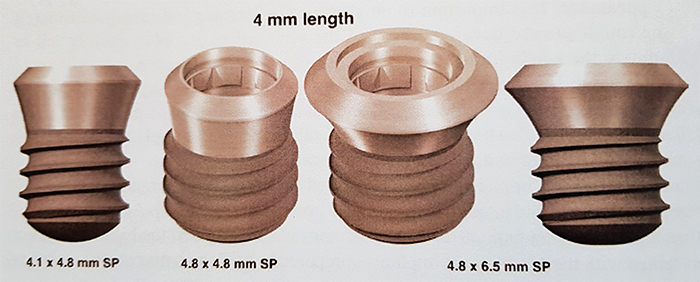
The main difference (other than having only 4 mm on the surface length), was that it has a thread pitch of 0.8 mm, instead of the 1.25 available on the 6-mm-long implant. It was launched commercially only in the Roxolid (Tltanium-Zirconium alloy), and in an SLActive surface, with the SP (Standard Plus) 1.8 polished collar neck, in three different configurations: 4. I (diameter) with 4.8 Neck (Regular Neck); 4.8 diameter with 4.8 neck (Wide-body), and 4.8 diameter with a 6.5 neck (Wide Neck
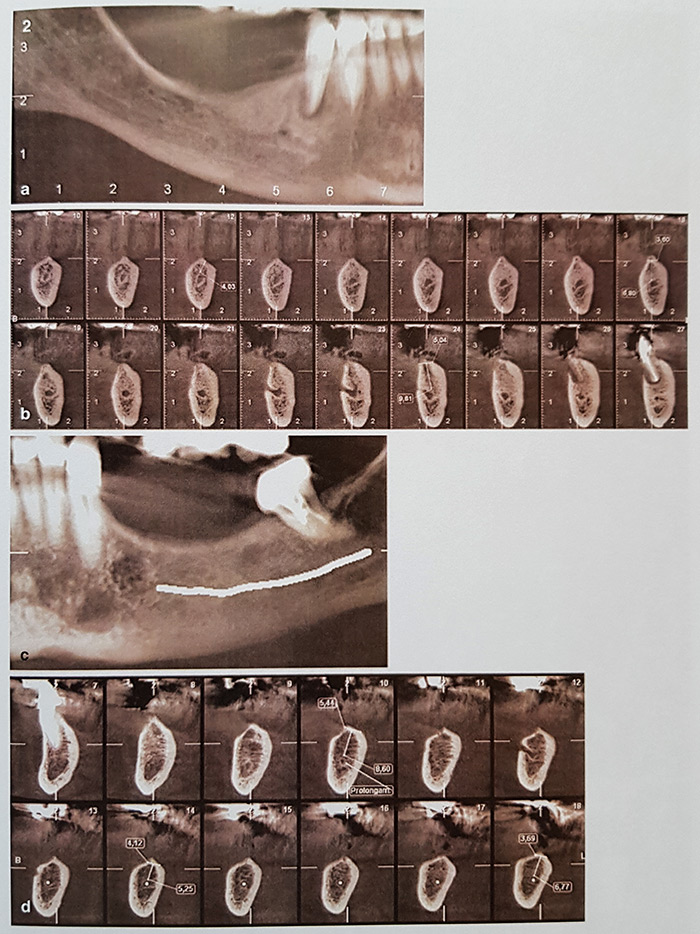
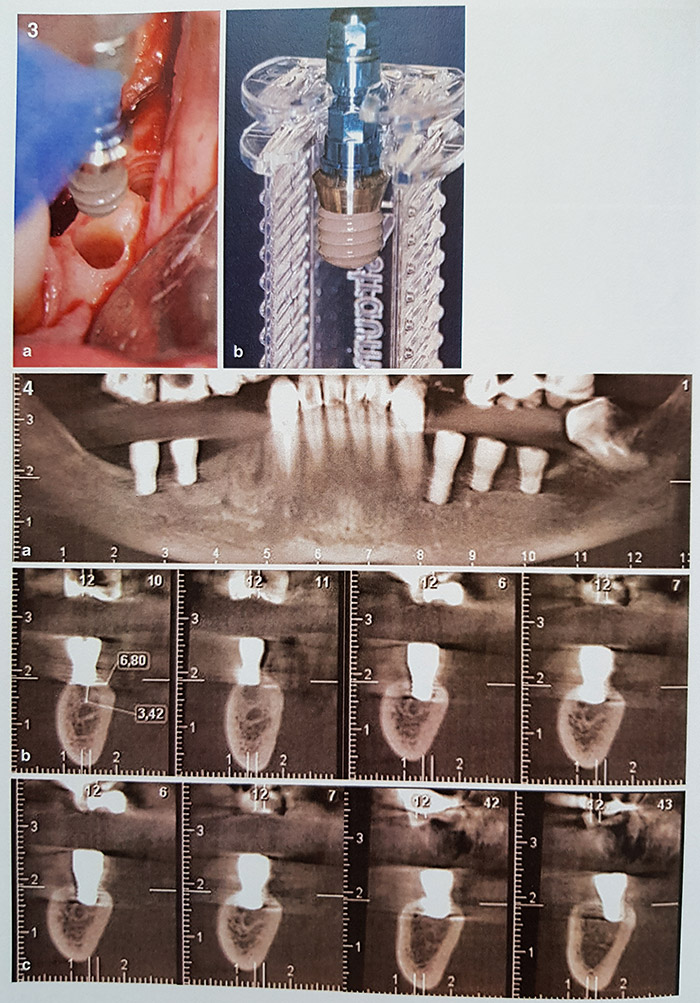
The same surgical steps are utilized, with a 4 mm mark present on all the drills and depth gauges. Extreme care should be taken to not overdrill the site in both vertical and horizontal directions, since it can lead to nerve damage and/or loss of primary stability. In the atrophic posterior mandible, usually all the alveolar is resorbed, and the implant has to be placed in a more cortical bone. Due to the reduced thread pitch, the primary stability obtained is very high. Hence, the use of tapping is highly recommended in order to avoid excessive insertion torque, which can potentially lead to lack of osseointegration.
A publication of Slotte et al, reported on 24 patients (87 implants) examined for 2 years post-loading. All implants were found to be stable [survival rate 95.7% (confidence interval, CI 88.8—98.3) after I year and 92.3% (Cl 84.5—96.2) after 2 years. The mean change from BL to 12 months was—O.43 mm (Cl 0.31—0.59; p <0.001 ) and from 12 to 24 month—0.11 mm (CI—0.01 p = 0.056).
The same group was followed for 5 years, and reported on a second publication, with 24 subjects and 71 implants still active at the 5-year follow-up (92.2% survival
Calvo-Guirado et al, reported on the use of forty 4 mm implants (4.1 x 4.8 RN, Roxolid, TIZi SLActive), placed in the posterior mandible of fully edentulous patients and splinted with longer (4.1 x 10 mm RN TiZi SLActive) implants to support a fixed prosthesis. After 1-year follow-up, the survival rate was 97.5%.
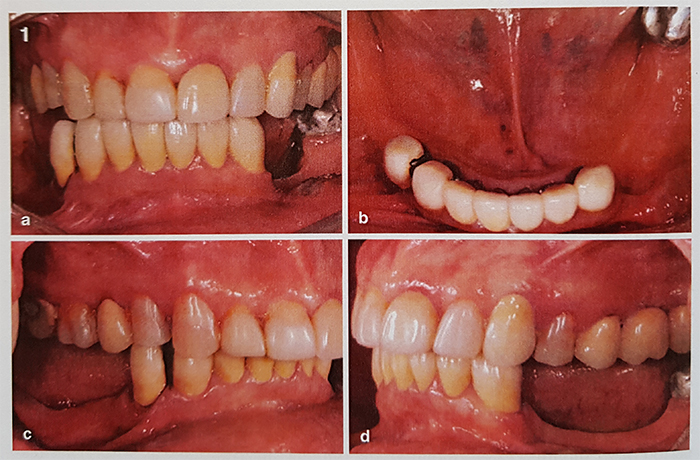
Polido and Nunes present the outcomes after 2 years of follow-up of 50 implants with 4 mm Of length placed in the posterior mandible of 25 patients. Implants were all titanium-zirconium SLActive surface, with 4 mm of length and 4.1 mm of diameter. Results showed that 5 out of the 50 implants failed in 4 patients. all before obtaining osseointegration (early failures). After an average follow-up period of 27 months (12—42 months), the implant survival rate was 90%. After restoration, no implants were lost, leading to a restoration survival rate of 100% of the restored implants. No patients reported neurosensory deficits.
The implant should be always splinted with another implant (of 4 mm or more in length). with flat occlusal surfaces. reduced occlusal area (premolarization). Good occlusal contacts and adjustment. and without cantilevers, in order to Obtain predictable results.
Slotte et al, conclude that with careful selection, treatment, and follow-up are carried out, 4-mm-long titanium implants, with the SLActive surface, can be safely and successfully used to support an FDP in severely resorbed posterior mandibles for at least 5 years. with healthy peri-imlplant conditions. Limited evidence is available for the use of this 4 mm implants for the posterior maxilla. However, Short implants may be considered a reasonable alternative for rehabilitation of severely resorbed maxillae with reduced height to avoid a more invasive and less predictable bone reconstruction before implant placement. Papaspyridakos and cols. performed a sistematic review and meta-analysis on the use of short implants (< 6 mm). Their clinical implications suggest the use of short implants as a valid alternative in selected cases where bone quantity precludes the use of longer implants. Which would potentially require extensive bone grafting that can increase morbidity and risks. they also point that short implants may be a viable alternative for the posterior mandible, where vertical augmentation tends to be a more challenging procedure.
The 4 mm implant is available on the European, south American, and occania markets since 2010, and although it has limited evidence published in the literature, it is considered a less invasive and more predictable alternative to restore the posterior region with better patient outcomes when compared to more invasive and less predictable vertical augmentation techniques specially For the mandible.
Conclusions
The surgical steps to place an ultrashort implant arc similar to those used to place a regular implant. and although they require a good level of surgical expertise to be placed, it is technically less demanding than any vertical augmentation technique.
The reported survival rate of 90—95% is lower than the average survival rate for regular length implants (>8mm). However, this procedure should compared with the more invasive surgical procedures routinely utilized for vertical augmentation of the posterior mandible that show a failure rate ranging from 20 to 70%. When native bone is available, the use of longer implants should be the first choice of treatment.
The use of the Straumann short (6 mm) has been extensively documented, with good long-term survival rates. Recently the ultrashort (4 mm) has also been the object of attention. and many clinical studies are currently underway, to assess the use of this interesting tool. The characteristics that contribute to the success of this implant are the excellent surface treatment (SLActive). applied at the novel Titanium-Zirconium alloy (Roxolid), and the well-documented tissue level polished collar neck design, that carries a strong and stable internal conical connection. Detailed restorative care and recommendations (should be used splinted, reduced (occlusal surface-premolarization. and low cusp occlusal tables) should be followed to optimize long-term results.
With the increasing trend to a minimally invasive surgical treatment with dental implants, especially with the elderly patients’ population, the Straumann short and ultrashort implants should considered when treating posterior vertically atrophic areas of the maxilla and the mandible. Current undergoing and future studies should bring long-term outcomes and stronger evidence for its use. specially for vertically deficient posterior mandibles.